Sciencemedicine
A 25-year Crohn’s disease mystery finally cracked by AI
KE
Kevin White
6 hours ago7 min read9 comments
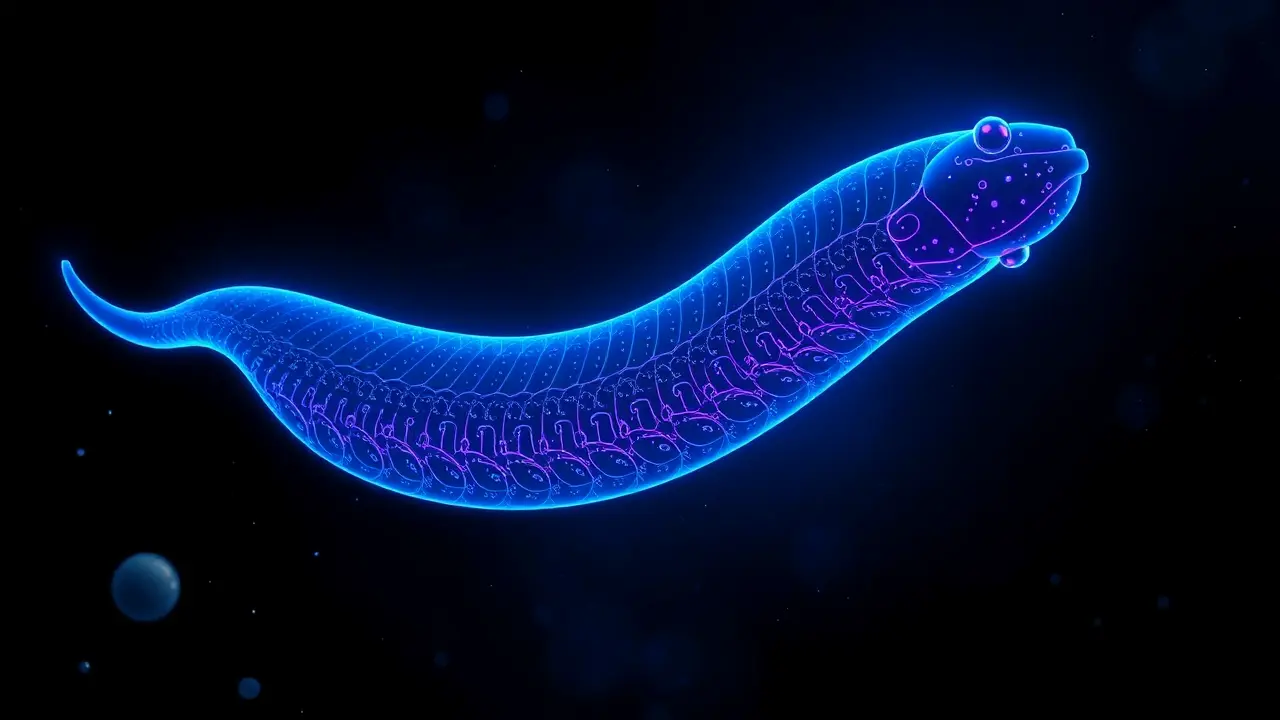
For a quarter of a century, the precise biological mechanism driving the debilitating inflammation characteristic of Crohn's disease has remained one of medical science's most stubborn enigmas, a complex puzzle where genetic predisposition and environmental triggers intersect in the gut's labyrinthine landscape. Now, in a landmark convergence of computational power and molecular biology, a research team from UC San Diego has finally cracked the code, deploying sophisticated artificial intelligence to illuminate a critical cellular decision-making process that governs intestinal health.Their investigation zeroed in on the gut's resident immune cells, the sentinels constantly patrolling the microbial frontier, and uncovered a fundamental molecular dialogue that dictates whether these cells initiate a controlled inflammatory response to a perceived threat or, conversely, activate pathways for tissue repair and healing. The research pinpointed a specific and crucial interaction between the NOD2 gene—long implicated in Crohn's susceptibility—and a structural protein known as girdin, revealing this partnership as the essential linchpin maintaining homeostatic balance in the intestinal lining.Think of NOD2 as a highly specialized sensor detecting bacterial components, while girdin acts as the molecular scaffold and signal translator; their handshake ensures a measured, appropriate immune response. However, the team's AI-driven analysis demonstrated that a common mutation in the NOD2 gene, found in a significant subset of Crohn's patients, severs this vital connection.Without girdin's regulatory influence, the inflammatory signals triggered by NOD2 spiral into a relentless, uncontrolled cascade, like a faulty alarm that cannot be silenced, leading to the chronic tissue damage and debilitating symptoms that define the disease. This discovery is monumental, shifting the paradigm from simply observing genetic associations to understanding the precise functional breakdown at a protein level.It opens up an entirely new therapeutic frontier: instead of broadly suppressing the immune system with drugs that carry significant side effects, future treatments could be designed to pharmacologically restore the NOD2-girdin interaction or mimic its calming signal, offering a targeted, mechanistic cure. This is the promise of next-generation medicine, where AI doesn't just analyze data but actively helps deconstruct the very architecture of disease, moving us from managing symptoms to engineering cures.The implications extend beyond Crohn's, potentially offering insights into other autoimmune conditions like ulcerative colitis and even broader inflammatory disorders, where similar breakdowns in cellular communication may be at play. The 25-year mystery is solved, and in its place, a new, hopeful chapter in biotech and precision medicine begins.
#
Stay Informed. Act Smarter.
Get weekly highlights, major headlines, and expert insights — then put your knowledge to work in our live prediction markets.
Related News
© 2025 Outpoll Service LTD. All rights reserved.