SciencemedicineRegenerative Medicine
Stanford makes stem cell transplants safer without chemo
KE
Kevin White
13 hours ago7 min read4 comments
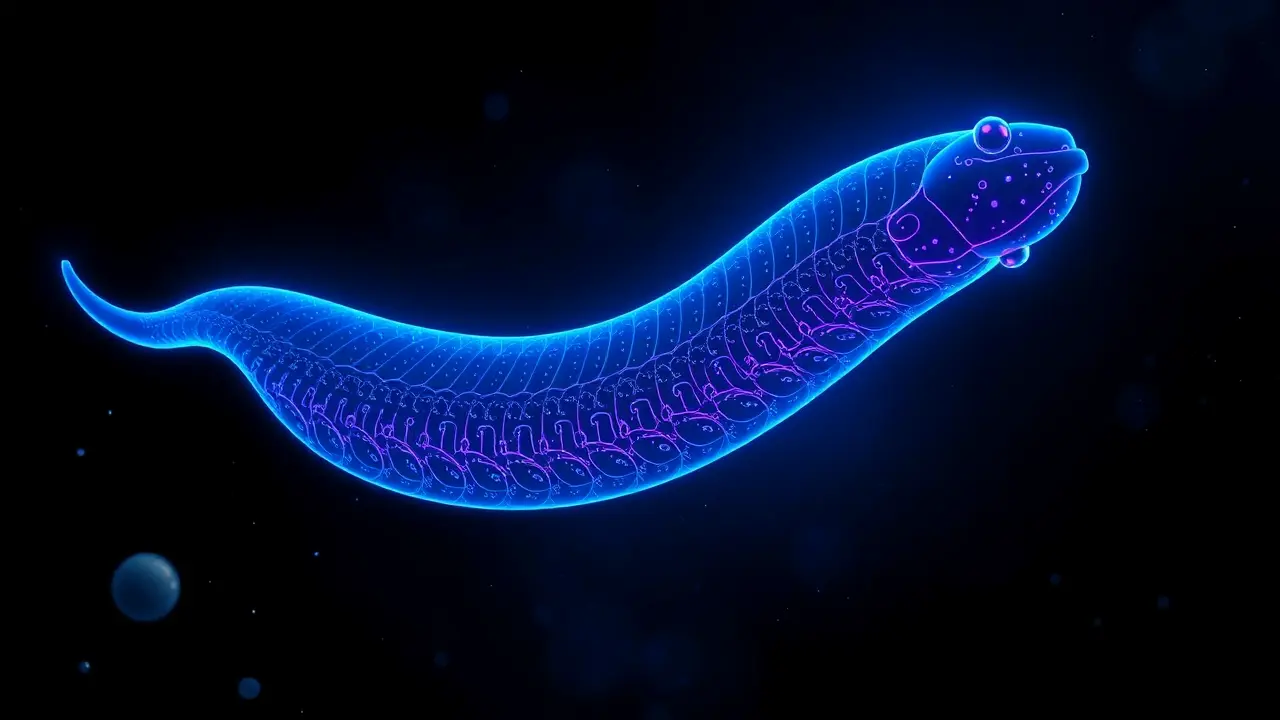
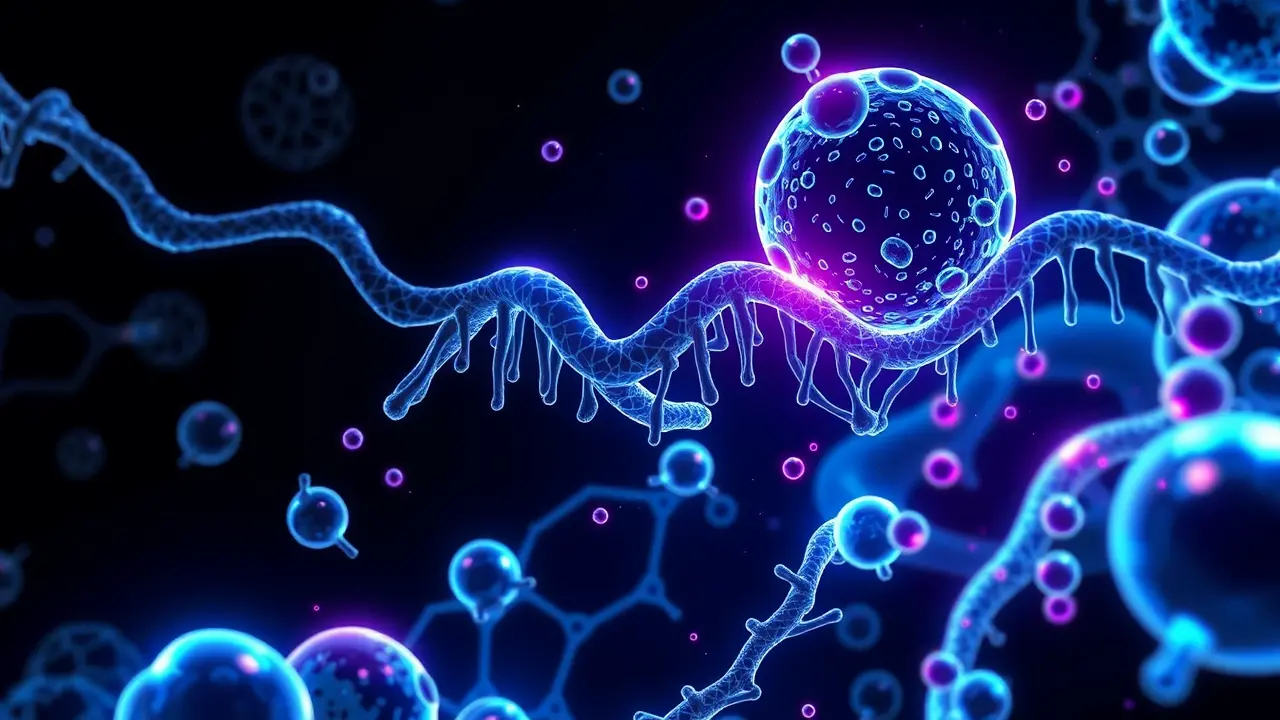
In a stunning leap forward for regenerative medicine that feels pulled from the pages of a sci-fi novel, a Stanford-led research consortium has fundamentally rewritten the playbook for stem cell transplantation. They've successfully replaced the brutal, toxic chemotherapy traditionally required before such procedures with an elegant, targeted antibody therapy, offering a lifeline to children suffering from Fanconi anemia—a rare and devastating genetic disorder that cripples the body's ability to repair its own DNA and often leads to bone marrow failure and a high risk of cancers.This isn't merely an incremental improvement; it's a paradigm shift. The old model was a scorched-earth campaign: using high-dose chemotherapy and full-body radiation to indiscriminately annihilate a patient's existing bone marrow stem cells, a process that creates a 'space' for healthy donor cells but at a horrific cost, causing organ damage, infertility, and secondary malignancies, with the procedure itself carrying a mortality risk.The new approach, however, is a precision-guided special ops mission. The key weapon is an antibody called briquilimab, which acts like a smart missile.It seeks out and latches onto a specific protein, CD117 (c-Kit), found abundantly on the surface of hematopoietic stem cells. By targeting this marker, briquilimab efficiently clears out the patient's own diseased and faulty stem cells, creating the necessary biological vacancy without the collateral devastation of chemo or radiation.The results from the initial clinical trial are nothing short of remarkable, demonstrating nearly complete donor cell engraftment—meaning the new, healthy stem cells from the donor took over the patient's blood and immune system with extraordinary efficiency. This level of chimerism, the coexistence of donor and recipient cells, is a critical metric for success, and achieving it without traditional conditioning is a historic first.Beyond the immediate safety benefits—dramatically reducing the risks of infections, organ toxicity, and long-term side effects—this methodology shatters previous limitations on donor eligibility. It opens the door for transplants from partially matched family members or even unrelated donors, a game-changer for patients from diverse ethnic backgrounds who have historically struggled to find perfect genetic matches in global registries.The implications ripple far beyond Fanconi anemia. The research team is already looking to deploy this briquilimab-based conditioning platform against a spectrum of other genetic blood disorders like sickle cell disease and beta-thalassemia, as well as for patients with other bone marrow failure syndromes.This represents the vanguard of a new era in biotech and cellular therapy, where the future of medicine is not about poisoning the body to save it, but about reprogramming and replacing its faulty systems with exquisitely targeted biological tools. It’s a future where the line between treatment and cure becomes increasingly blurred, and where the once-unimaginable prospect of a gentle transplant is now a clinical reality.
#featured
#stem cell transplant
#Fanconi anemia
#briquilimab
#chemotherapy-free
#donor cells
#medical breakthrough
Stay Informed. Act Smarter.
Get weekly highlights, major headlines, and expert insights — then put your knowledge to work in our live prediction markets.
Related News
© 2025 Outpoll Service LTD. All rights reserved.