SciencemedicineRegenerative Medicine
Scientists turn body fat into bone to heal spinal fractures
KE
Kevin White
3 hours ago7 min read1 comments
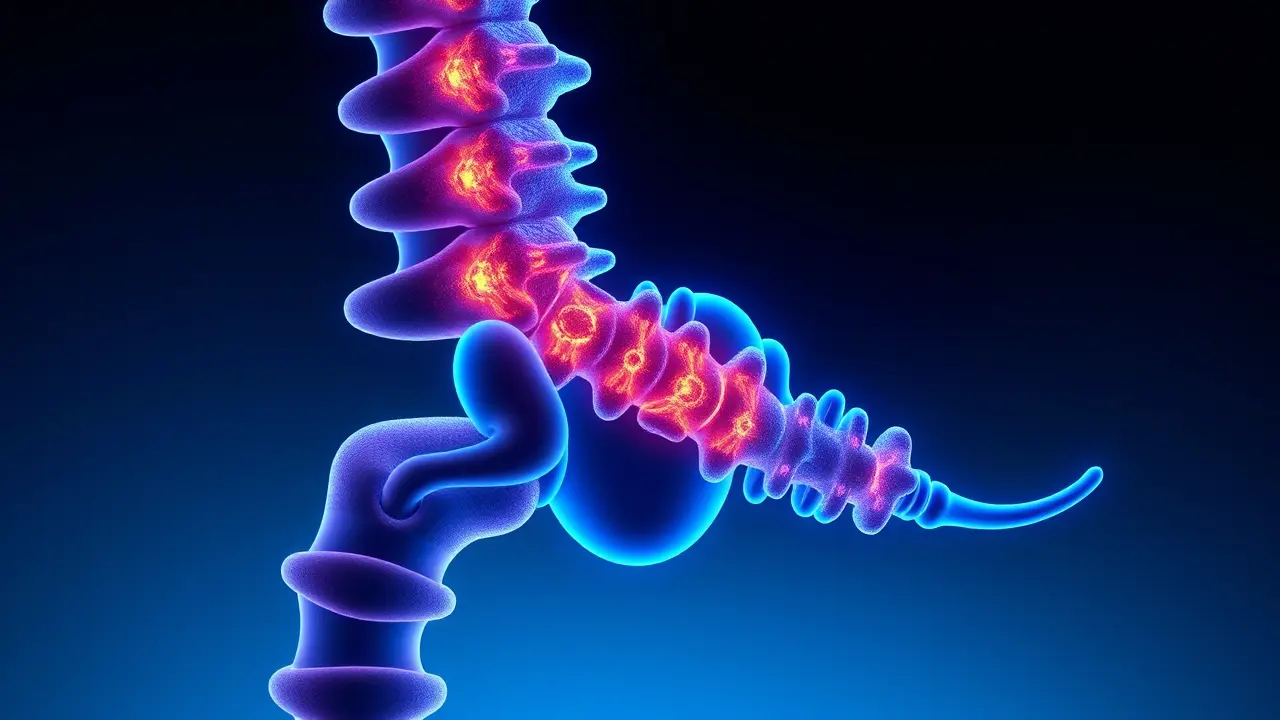
In a development that reads like a page from a near-future medical thriller, scientists at Osaka University have successfully engineered a process to transform ordinary body fat into functional bone tissue, demonstrating its efficacy in healing spinal fractures in rodent models with a level of precision that could fundamentally reshape orthopedic and regenerative medicine. This isn't merely a minor procedural improvement; it's a paradigm shift that leverages the body's own abundant and easily accessible adipose tissue as a veritable gold mine of mesenchymal stem cells (MSCs), which possess the remarkable, pluripotent ability to differentiate into bone, cartilage, and fat.The researchers' ingenious methodology involved harvesting these stem cells from fat, a far less invasive and painful procedure than traditional bone marrow aspiration, and then coaxing them in vitro to form three-dimensional, bone-forming clusters known as spheroids. These spheroids were then paired with a bio-ceramic material called β-tricalcium phosphate, a scaffold that mimics the natural mineral component of bone, creating a powerful, synergistic implant.When this bio-hybrid construct was applied to spinal fractures in rats—specifically modeled to mimic the debilitating compression fractures caused by osteoporosis—the results were profound: the animals not only healed but regenerated stronger, denser, healthier vertebral bone, effectively reversing the structural damage. The implications for human medicine are staggering.Osteoporosis, a silent epidemic affecting hundreds of millions globally, primarily postmenopausal women and the elderly, leads to fragile bones and an estimated 8. 9 million fractures annually worldwide, with spinal fractures causing chronic pain, loss of height, and a severe reduction in quality of life.Current treatments range from pain management and bracing to invasive surgical procedures like vertebroplasty, which involves injecting bone cement, but these are often palliative rather than regenerative and carry risks of their own. The Osaka approach offers a tantalizing alternative: a one-step, minimally invasive, autologous (using the patient's own cells) therapy that doesn't just patch the fracture but actively stimulates the body's innate healing mechanisms to rebuild it from within.This dovetails perfectly with the accelerating field of biotech and CRISPR-based genetic therapies, moving us from a era of mechanical repair to one of biological regeneration. Imagine a future clinic where a patient with a spinal injury undergoes a simple liposuction procedure; their extracted fat is processed in an on-site bioreactor to create personalized bone grafts, which are then implanted in a same-day procedure, drastically reducing hospital stays and infection risks.Of course, the path from rat models to human clinical trials is fraught with challenges, including scaling up the production of these stem cell spheroids, ensuring their long-term stability and integration, and navigating complex regulatory hurdles. Yet, the work in Osaka represents a critical proof-of-concept, a beacon pointing toward a future where we can harness our own biological resources to combat the ravages of age and disease, turning what was once considered mere excess—body fat—into the very building blocks of a stronger skeletal framework.
#featured
#stem cells
#spinal fractures
#osteoporosis
#regenerative medicine
#medical research
#bone healing
#Osaka
Stay Informed. Act Smarter.
Get weekly highlights, major headlines, and expert insights — then put your knowledge to work in our live prediction markets.
Related News
© 2025 Outpoll Service LTD. All rights reserved.