SciencemedicineCancer Research
A New Light-Based Cancer Treatment Kills Tumor Cells and Spares Healthy Ones
KE
Kevin White
21 hours ago7 min read3 comments
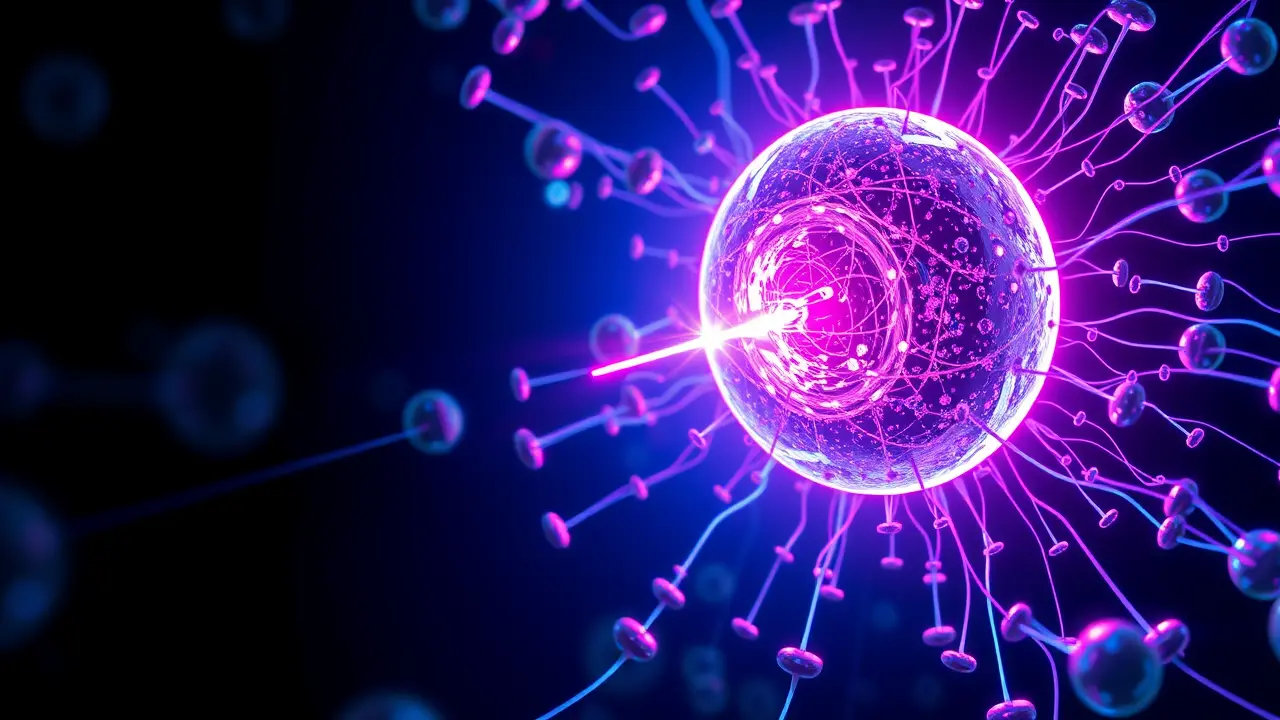
In a development that feels ripped from the speculative pages of a Neal Stephenson novel, a consortium of international researchers has engineered a paradigm shift in oncology by weaponizing light itself. This isn't science fiction; it's a clinically validated therapy that leverages the precise interplay of LED technology and bespoke nanomaterials to hunt cancer cells with a sniper's discretion, sparing the healthy tissue that conventional treatments like chemotherapy and radiation so often ravage.The core innovation lies in a class of nanoparticles, engineered to act as thermal Trojan horses. These microscopic agents are administered and, through various targeting mechanisms, preferentially accumulate within the tumor microenvironment.When exposed to a specific wavelength of light delivered via external or even implantable LED arrays, these particles undergo a phenomenon known as localized surface plasmon resonance, converting photonic energy into intense, hyper-localized heat. This isn't a blanket scorching of the body; it's a cellular-level thermal ablation, where malignant cells are literally cooked from the inside out, reaching lethal temperatures of 42-45°C (107-113°F), while the surrounding, nanoparticle-free healthy tissues remain completely unaffected, their cellular machinery undisturbed.The elegance of this approach is a direct affront to the blunt-instrument legacy of cancer care. For decades, the field has been trapped in a brutal trade-off: effective tumor destruction at the cost of systemic toxicity.Chemotherapy, a chemical war of attrition, and radiotherapy, a controlled bombardment, are fundamentally indiscriminate, leading to the debilitating side effects—neutropenia, neuropathies, organ damage—that define the cancer patient's ordeal. This new photothermal therapy (PTT), however, belongs to the burgeoning era of theranostics—a portmanteau of therapy and diagnostics—where treatment is diagnostic, targeted, and minimally invasive.The nanomaterials themselves are often multifunctional; some are tuned to also act as contrast agents for imaging techniques like MRI or photoacoustic tomography, allowing clinicians to visualize the tumor, confirm the successful homing of the nanoparticles, and then, with the flip of a switch, activate their destructive potential, creating a closed-loop 'see and treat' system. The historical precedent for light in medicine, photodynamic therapy (PDT), relies on photosensitizing chemicals that produce reactive oxygen species upon light activation, but its efficacy is limited by oxygen dependence and poor tissue penetration of light.This new thermal approach sidesteps those limitations, offering a more robust and direct mechanism of action. The implications for hard-to-treat cancers, particularly those nestled near critical structures like the brainstem or major nerves, are profound.Imagine a glioblastoma patient receiving an intratumoral injection of these nanoparticles, followed by a session under a focused light source, emerging with the tumor neutralized and cognitive functions fully intact. Or consider its application in metastatic disease, where numerous, scattered microtumors could be systematically targeted without subjecting the patient to whole-body toxicity.The road to widespread clinical adoption is, of course, paved with challenges. The long-term biocompatibility and clearance pathways of these engineered nanomaterials must be exhaustively characterized to avoid new iatrogenic diseases.Scaling up the synthesis of clinical-grade nanoparticles to meet global demand presents a significant manufacturing hurdle. Furthermore, the depth of light penetration in human tissue, while improved with near-infrared wavelengths, remains a physical constraint, though this is being addressed with the development of fiber-optic and endoscopic delivery systems for deep-seated tumors.Financially, the therapy could initially be costly, but if it reduces or eliminates the need for lengthy hospital stays, supportive care for side effects, and management of long-term treatment sequelae, it may prove economically transformative for healthcare systems. Ethically, it forces a re-evaluation of the risk-benefit calculus in oncology, potentially making previously inoperable or untreatable cancers manageable chronic conditions.As Dr. Alena Petrov from the Institute for Bionanotechnology remarked in our correspondence, 'We are not just adding another tool to the oncology toolkit; we are fundamentally redefining the relationship between the treatment and the patient's body.The goal is no longer just survival, but survival with quality of life. ' This breakthrough stands as a testament to the power of interdisciplinary convergence—where materials science, optical engineering, and molecular biology collide to create solutions that are as elegant as they are effective, heralding a future where the fight against cancer is no longer a scorched-earth campaign, but a series of precise, decisive, and mercifully gentle strikes.
#featured
#cancer treatment
#light-based therapy
#nanomaterials
#LED technology
#localized heat
#tumor cells
Stay Informed. Act Smarter.
Get weekly highlights, major headlines, and expert insights — then put your knowledge to work in our live prediction markets.
Related News
© 2025 Outpoll Service LTD. All rights reserved.